Management of alopecia in skin of color is challenging due to a paucity of research into its pathophysiology coupled with a poor understanding of the basic hair care practices in this patient population. For the patient, it is often associated with severe emotional distress. Unfortunately, many forms of hair loss are refractory to standard therapies.
At the 2020 Skin of Color Virtual Update, Dr. Crystal Aguh highlighted emerging therapies for various forms of alopecia in skin of color as our understanding of these conditions continue to unfold.
Central Centrifugal Cicatricial Alopecia (CCCA) is the prototypical form of hair loss in black women. It is a progressive form of scarring alopecia where fibrosis, not inflammation, is the predominant finding. The literature supports preferential expression of fibroproliferative genes in patients with CCCA. In fact, Dr. Aguh’s group demonstrated that PRKAA2, a gene that encodes for adenosine monophosphate kinase (AMPK), was under-expressed by a 1/3 in CCCA scalp samples.
So why metformin?
Reduced activity of AMPK is also implicated in the pathogenesis of hepatic fibrosis and idiopathic pulmonary fibrosis. In mouse model of IPF, metformin was found to reverse and accelerate resolution of the fibrotic processes via deactivation and apoptosis of myofibroblasts through AMPK activation.
-
- Dosage: 10-20% Topical Metformin compounded in lipoderm once daily.
- At that concentration, there is limited systemic absorption.
- Main side effects are scalp dryness and irritation. Dr. Aguh recommends applying light oil (olive or Jojoba) coat to scalp to help with irritation and dryness.
- It works 10-15 % of the time.
Another form of alopecia that disproportionately affects women is Lichen planopilaris (LPP). LPP is an inflammatory form of primary scarring alopecia. Signs of clinical activity include follicular hyperkeratosis, perifollicular erythema, and loss of follicular ostia. Patients also report loss of body hair. Meanwhile frontal fibrosing alopecia (FFA) is a subtype of lichen planopilaris characterized by slow recession of the frontal and bitemporal hairline. Dr. Aguh highlighted two adjunctive options for the treatment of LPP and FFA for patients who have failed standard therapies.
-
-
Naltrexone
-
-
- mu-opioid receptor antagonist currently FDA approved for the treatment of opioid and alcohol dependence. In dermatology, it has been used off-label for the treatment of pruritus and as an anti-inflammatory agent.
- It is hypothesized that lower than standard doses of naltrexone inhibits cellular proliferation of T and B cells and block Toll-like receptor 4, resulting in an analgesic and anti-inflammatory effect.
- In one case series of four patients with LPP, use of naltrexone led to reduction in symptoms of pruritus, clinical evidence of inflammation of the scalp, and disease progression.
- Dose: 3 mg daily
- Drawback: 3 mg pills have to be compounded as the standard pill comes in 50 mg.
-
-
3% Tacrolimus cleanser (in Cetaphil cleanser)
-
-
- Tacrolimus is a commonly anti-inflammatory agent for inflammatory skin conditions including lichen planopilaris.
- Higher strengths of tacrolimus can be compounded to improve efficacy.
- One retrospective study demonstrated that patients treated with 0.3% tacrolimus were significantly more likely to stabilize in 3 months compared with patients treated with clobetasol/betamethasone.
- Drawback: very expensive. It costs about $120 for 30 ml of cleanser.
Acquired Trichorrhexis Nodosa (ATN) is a recurrent hair breakage that occurs as a result of damaging hair practices. Common culprits include chemical relaxers, thermal styling, and hair coloring. Patients will often complain of lack of hair growth. It can involve all parts of the scalp but nape of the neck is often affected. Dr. Aguh’s stressed that proper hair care is key for successful treatment. She proposed the following regimen for curly damaged hair:
-
- Apply protein treatment to dry or damp hair. Cover with shower cap or heating source for 30 minutes.
- Wash hair once weekly with gentle shampoo (sulfate-free or containing a gentle sulfate)
- Deep condition with every shampoo. Follow deep conditioning with moisturizing rinse-out conditioner.
- Add leave in conditioner after washing, at least 3x/week. Glycerin based leave in conditioners can be especially helpful for very dry hair
- End washing session with light oil.
Traction Alopecia is another very common form of hair loss, especially in black women. It is likely due to the curly hair type, intrinsic low density of the hair at baseline as well as hairstyle practices. Dr. Aguh found that oral minoxidil, in lieu of topical minoxidil, is very effective for this type of hair loss.
Oral minoxidil
-
- Potent hypertensive that can lead to hair regrowth even at low doses.
- In a case series of 18 patients with Androgenetic Alopecia or Traction Alopecia treated with 1.25 mg minoxidil daily, among all patients (9/18) who regularly recorded blood pressure, only 1 reported hypotensive symptoms. No cardiac events were noted. Five of 18 patients reported increased scalp hair at this dose, 7/18 reported facial hypertrichosis.
- Side effects of minoxidil (at 5-40 mg dosing) include weight gain, headache, hypotension, tachycardia. Rare but serious side effects include SJS/TEN, CHF, pericarditis.
- No serious side effects yet reported at lower doses.
- Dosage: alternative dosing strategies:
-
-
- 625 mg then increase to 1.25 mg then to 2.5 mg (over the course of a month)
- 25mg then increase to 2.5mg (over the course of a month)
-
-
- Avoid in pregnant women, patients with low BP, CHF.
The relatively new kid on the block is platelet-rich plasma (PRP) for various forms alopecia. PRP is an option for the right patient with scarring alopecia, such as CCA and LPP.
Dr. Aguh’s PRP protocol
-
- 3-4 treatments space 3-4 weeks apart.
- If the patient is already on minoxidil, she continues it.
- If they are not on minoxidil, she does not start until the PRP is done to avoid the initial shedding phase of minoxidil.
- Discuss discontinuation of treatment with patient if no improvement is seen after two sessions
She emphasized that the results of PRP are temporary. At about one year, repeat PRP treatments are required to obtain similar results.
Alopecia can be distressing, frustrating, and even embarrassing. Many patients seek ways to camouflage (i.e., by wearing a wig) instead of seeking appropriate dermatologic care. Dr. Aguh’s demonstrated successful treatment of various forms of alopecia with the aforementioned adjunctive therapies. Next time you see a skin of color patient with alopecia, Dr. Aguh’s recommends asking yourself “Are your treatment options going to move the patient out of the wig?”
This information was presented by Dr. Aguh at the 2020 Skin of Color Update Virtual conference held on September 13, 2020.
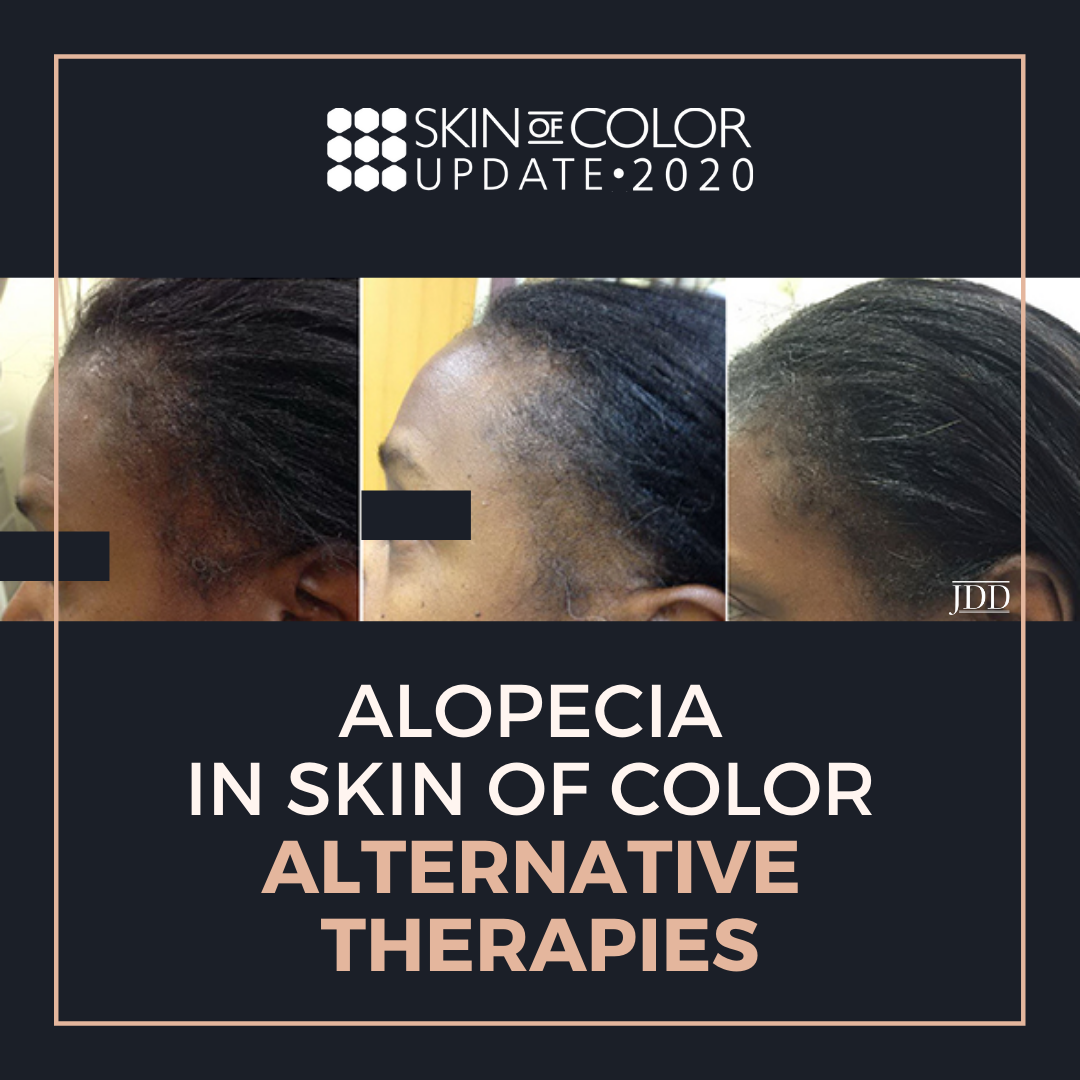
Photo credit: Image used with permission from the Journal of Drugs in Dermatology.
Did you enjoy this article? Find more on Skin of Color here.