Wow! The ODAC Dermatology Conference in January 2022 highlighted the importance of conference attendance and the need for expert lectures on clinically relevant dermatologic topics. We are in an era when basic sciences and translational research has direct correlation and impact on our therapeutic measures for patients. While it is refreshing to have so many options for patients’ treatment, it can also be daunting! With the help of experts such as Dr. Adam Friedman, we can appreciate the translational research that helps guide our more practical approaches to treatment in the clinic setting. During the conference, Dr. Friedman provided attendees a comprehensive overview on the pathophysiology of pruritus (itch), its impact on patients’ quality of life, and detailed treatment options based on the specific underlying cause.
Historically, pruritus treatment included a hodgepodge of therapeutic measures that were NOT grounded in any specific study or pathophysiologic pathway. This led to inadequate symptom and disease management and as a result left both patient and provider frustrated. Rarely are moisturizers and over the counter oral antihistamine the answer for pruritus management.
Why does all this matter? Well, because we want to help patients feel better! Pruritus alone can lead to many other frustrating symptoms and complications including:
-
- Irritability
- Stress
- Anxiety
- Insomnia —-> Fatigue
- Suicidal ideation
To better understand how to control pruritus it is important to appreciate the key players of our immune system that affect this symptom and cutaneous disorder. Remember from our days of book learning the importance of macrophages, neutrophils, eosinophils, mast cells, Th2-CD4 cells and keratinocytes (skin-specific cells). So why is this important when a patient presents to the clinic with bothersome or debilitating pruritus? It is important because we need to appreciate if this is due to a primary inflammatory versus primary neurogenic-induced itch. And it is best to think of this on a spectrum as outlined below:
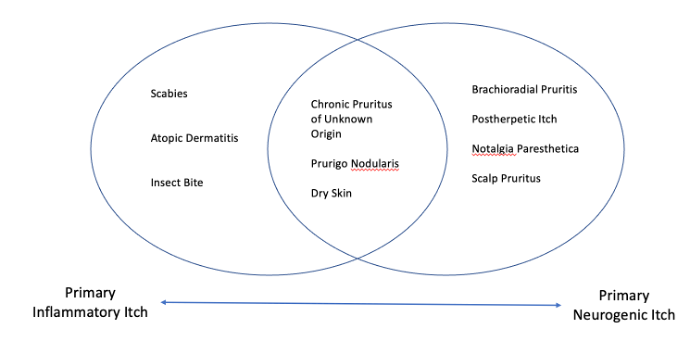 There is a myriad of inflammatory and neurogenic processes that induce pruritus as a symptom. In a subset of patients, pruritus is the primary etiology. Itch requires treatment regardless of whether it is the primary or secondary condition.
There is a myriad of inflammatory and neurogenic processes that induce pruritus as a symptom. In a subset of patients, pruritus is the primary etiology. Itch requires treatment regardless of whether it is the primary or secondary condition.
A six-week cut off, akin to urticaria, has been designated to distinguish between acute and chronic pruritus. While this has been delineated as the duration, providers should work-up and treat pruritus based on their clinical assessment, physical exam findings, review of systems, pertinent risk factors and age-appropriate screening parameters. Dr. Friedman focused on the algorithm published in the Journal of the American Academy of Dermatology (JAAD) in January 2022 to provide a road map for what our clinical assessment and work-up should be when addressing chronic pruritus.
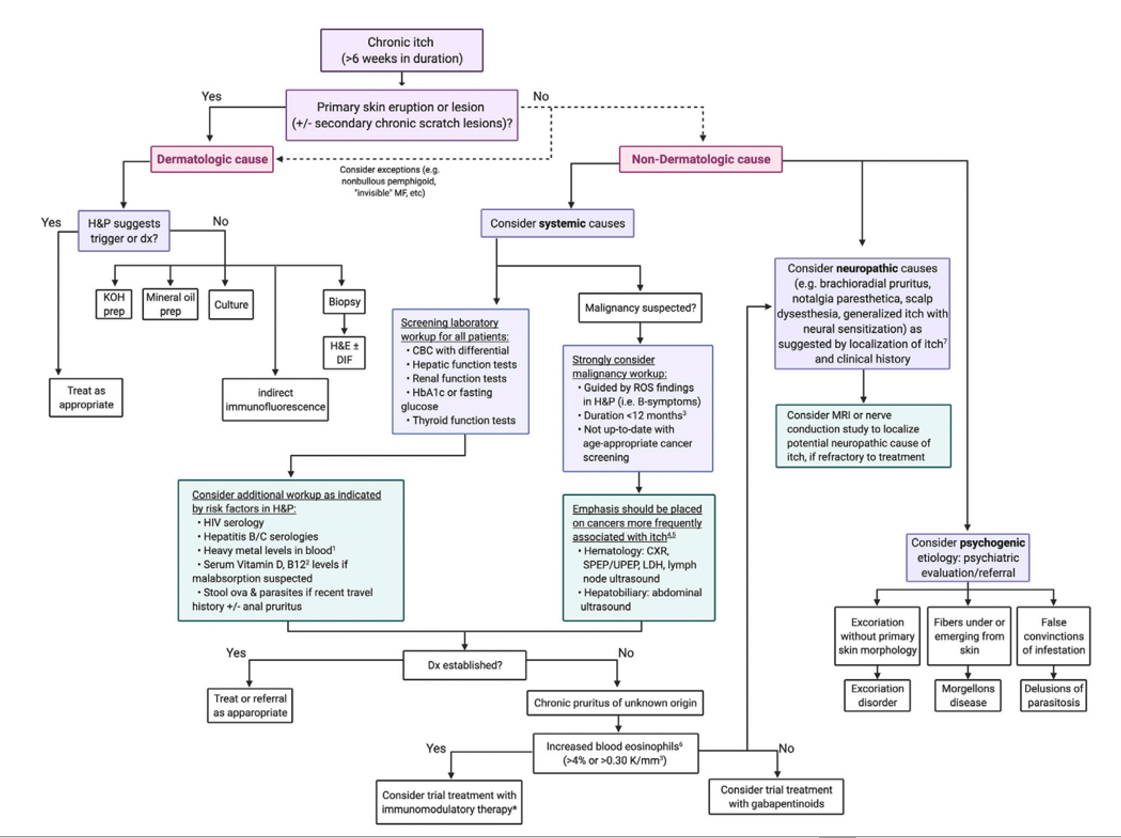
While the above recommendations may seem daunting, they are not meant to be! Take a deep breath and review it once or twice and you will have a better appreciation for how to provide a comprehensive assessment for most of our patients!
One’s initial assessment does NOT need to incorporate every laboratory test, but it is important to obtain a comprehensive history, risk factors and physical exam. Once this is done, the initial work-up should include:
-
- Complete Blood Count (CBC) w/DIF
- Comprehensive Metabolic Panel (CMP)
- Thyroid function testing (TSH)
- Chest X-ray
- Stool ova/parasites (***especially with anogenital pruritus)
Every patient should be counseled on the importance of a gentle skin care routine, especially the elderly population! Some basic suggestions to keep in mind, include the following:
-
- Use of non-alkaline soaps and moisturizers
- Soft cotton clothing when appropriate
- Lukewarm water when bathing
And advise to avoid the following when possible:
-
- Frequent bathing
- Heat
- Dry climate
- Alcohol
- Spicy foods
Furthermore, do not recommend antihistamines as they are NOT effective for chronic pruritus. Instead, it leads to more side effect profile of drowsiness without any real benefit.
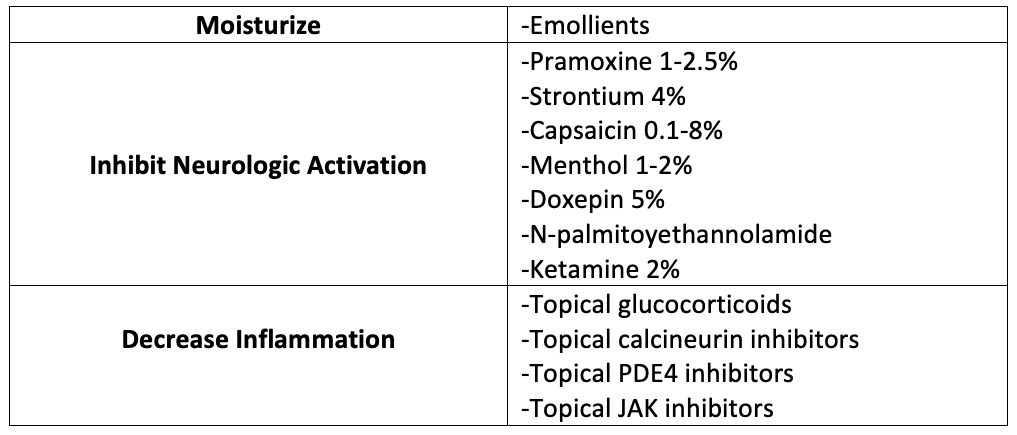
When it comes to treatment of pruritus, one can consider the use of topicals and systemic therapies based on the patient’s symptoms, underlying etiology, risk factors and co-morbidities. For topical treatment options, consider the following:
 As for systemic therapy, do not forget about narrow band UVB therapy! It is highly effective in the correct patient population as it can be helpful in a myriad of inflammatory cutaneous diseases associated with pruritus such as psoriasis, atopic dermatitis, cutaneous T-cell lymphoma, lichen planus and even chronic spontaneous urticaria. It is also relatively safe in patients with multiple, life-threatening diseases such as end stage renal disease, hepatitis C and primary biliary cholangitis.
As for systemic therapy, do not forget about narrow band UVB therapy! It is highly effective in the correct patient population as it can be helpful in a myriad of inflammatory cutaneous diseases associated with pruritus such as psoriasis, atopic dermatitis, cutaneous T-cell lymphoma, lichen planus and even chronic spontaneous urticaria. It is also relatively safe in patients with multiple, life-threatening diseases such as end stage renal disease, hepatitis C and primary biliary cholangitis.
While it is overwhelming to think about, there are many treatment options available to provide relief of pruritus for patients. It can be easy to altogether avoid systemic therapies, but they can provide a great deal of relief to patients. To make sense of all these options consider the following categories and possible options:
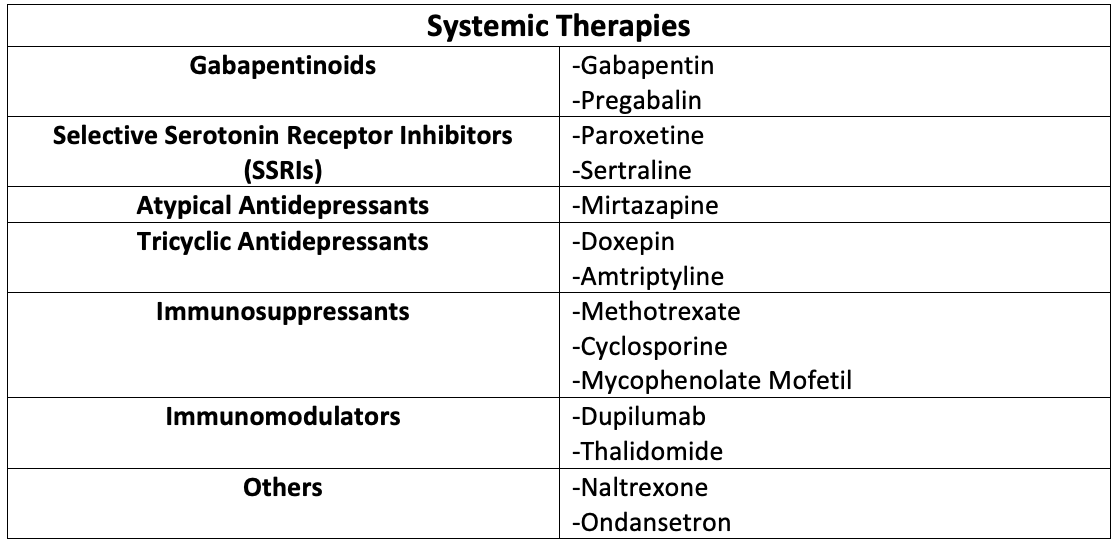 When choosing any of the above therapies it is best to start slow and titrate accordingly based on co-morbidities, renal clearance, any underlying hepatic dysfunction, or drug-drug interactions.
When choosing any of the above therapies it is best to start slow and titrate accordingly based on co-morbidities, renal clearance, any underlying hepatic dysfunction, or drug-drug interactions.
For gabapentin, we can increase to a total of 3600 mg per day divided into three times per day dosing; however, renal clearance must be taken into consideration with this medication.
When it comes to mirtazapine, again, start at 15 mg dose and administer in the evening due to concern for drowsiness. If it is not too sedating, one can decrease to 7.5 mg nightly (shown to be cause more sedation than the 15 mg dosing). Make note of the black box warning for suicidality and consider weight gain for certain patients.
Another non-FDA approved therapy for chronic pruritus that has shown great efficacy is naltrexone, a mu opioid receptor antagonist. The dosing can range from 12.5-50 mg daily, but an important contraindication is that patients cannot be on any opioid analgesic. Common side effect profile for this medication includes nausea, headache, dizziness, nervousness, fatigue, insomnia, joint and muscle pains. However, it is very effective for pruritus associated with cholestasis, atopic dermatitis, prurigo nodularis, and lichen simplex chronicus.
An important game changer for chronic pruritus has become dupilumab an anti-IL4 alpha receptor antagonist. Its mechanism of action inhibits IL-4 and IL-13 cytokine induced responses. While initially used for atopic dermatitis, clinicians have found it just as helpful for prurigo nodularis and chronic itch of unknown etiology.
The greatest takeaway of Dr. Friedman’s talk was that there is a light at end of the tunnel! We have a plethora of options to treat chronic pruritus. It is our responsibility as clinicians to recognize this debilitating cutaneous condition to ensure a proper multimodal treatment plan is implemented.
This information was presented by Dr. Adam Friedman at the 2022 ODAC Dermatology, Aesthetic and Surgical Conference held January 14-17, 2022. The above highlights from her lecture were written and compiled by Dr. Freba Farhat.
Did you enjoy this article? You can find more on Medical Dermatology here.