Dermatophytosis constitutes a big chunk of “bread and butter” in dermatology. In fact, an average of 4.1 million visits a year were due to dermatophytosis from 1995 to 2004! Nevertheless, these fungi can still stump the most seasoned dermatologist, and misdiagnosis can be surprisingly common. Dr. Adam Friedman, Professor, Interim Chair, and Program Director of Dermatology at George Washington School of Medicine and Health Sciences, recently presented interesting cases and practical pearls on how to diagnose and treat dermatophytosis. Here are some highlights.
Make the Diagnosis
Here’s the golden rule: if there is scale, scrape it!
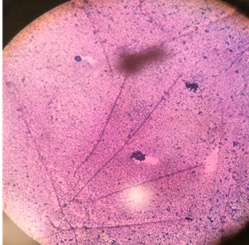
KOH preparation is first line in diagnosis of dermatophytosis. Do you follow this rule? A recent survey showed that the percentages of dermatologists who scrape when suspicious of dermatophytosis were only 20-30% (always) and 30-40% (very often). Next, histology can be helpful in diagnosing nail fungus and Majocci’s granuloma (where KOH is usually negative). Fungal culture be helpful to guide anti-fungal therapy, especially for tinea capitis in children.
Tinea Pedis
Tinea pedis is the most common form of skin fungal infection, and there are 4 types: moccasin, interdigital, bullous, and ulcerative.

Don’t forget that non-dermatophytes (S. dimidiatum; S. hyalinum) can cause identical findings! Also, an exuberant dermatophytid (or “id”) reaction, an inflammatory response to the fungal infection, can accompany findings of dermatophytosis. When you see a 2-hand-1-foot (or vice-versa) involvement, this can be another clue for diagnosing tinea pedis.
While topical azoles (econazole, other azoles) and allylamines (terbinafine, naftifine) and antifungal powder/spray weekly to shoes have been the mainstay treatment, there are some new topical options available. Luliconazole 1% cream (daily for 2 week) for moist macerated web space; naftifine 2% gel and cream (daily for 2 week) for dry, scaling plaques; and urea 40% cream for moccasin tinea pedis have shown efficacy.
What about systemic anti-fungal therapy? The moccasin type and vesicular type may warrant oral terbinafine 250mg BID for 2-6 weeks and 2 weeks, respectively. Since the vesicular type may have superimposed bacterial infection, an oral antibiotic may also be considered.
Tinea Manuum
Nails are often affected, and recurrence is frequent. Therefore, oral anti-fungal therapy is warranted for tinea manuum.

Junk by the Junk: Tinea Cruris

Often sparing the scrotum and penis, tinea cruris occurs more commonly in men. Keep a degree of suspicion for mimickers of tinea cruris—inverse psoriasis, intertrigo, benign familial pemphigus, and erythrasma (grab that Wood’s lamp!)!
Tinea Capitis

Tinea capitis can present as non-inflammatory (black dot, seborrheic), inflammatory (kerion), or both. When inflammatory, perform both fungal and bacterial culture and include an anti-inflammatory component in the treatment plan.
Of course, systemic treatment is required for tinea capitis, as follows:
- Griseofulvin is better for canis
Dose at 20mg/kg for eight weeks or at least 2 weeks past no further symptoms. If micronized, 15-25mg/kg daily is recommended; if ultramicronized, 10mg/kg daily is recommended. A single dose can be given with a fat-containing meal.
- Terbinafine is better for rubrum
If less weighing less than 20kg, dose at 62.5mg daily for 6 week.
- Combine above systemic therapy with ketoconazole 2% shampoo (leave on scalp for 5 minutes before rinsing)
- Re-culture at 1 month to ensure response to treatment!
Tinea Unguium

About 50% of all nail dystrophy is due to fungus (and 90% of that is due to dermatophytes). Therefore, always look for coinciding tinea pedis, and know the differential diagnosis – allergic contact (nail polish, food items), candida chronic paronychia, psoriasis, lichen planus, nail dystrophies (ie, nephrogenic), drugs, and malignancy!
The most common treatment is terbinafine (250mg daily for 6 weeks for fingernails and 12 weeks for toenails). Other options include itraconazole (400mg a week for 6 weeks for fingernails and 12 weeks for toenails) and fluconazole (300-450mg a week for 6 months for fingernails and 9 months for toenails). Non-response or recurrence may occur in severe disease, non-dermatophyte infection, host factors (immunosuppression, PVD, poorly controlled diabetes), or wrong diagnosis.
Now, are you ready for a mind-blowing fact?
What does this mean? Empiric treatment with terbinafine may be more cost-effective than confirmatory testing with minimal effect on safety, although this is against AAD guidelines. Confirmatory testing before efinaconazole will reduce costs across a range of disease prevalence. As hepatic risk for terbinafine is merely one in 50,000 to 120,000, the practice is now trending away from routine monitoring. What is your practice?
Hopefully, this inspires you to go out and fight the fungus among us!
This information was presented by Dr. Adam Friedman at the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference held January 18th-21st, 2019 in Orlando, FL. The above highlights from his lecture were written and compiled by Dr. InYoung Kim, one of the 5 residents who participated in the Sun Resident Career Mentorship Program (a program supported by an educational grant from Sun Pharmaceutical Industries, Inc.).
Image Credits:
Figure 1A: Courtesy of Adam Friedman, MD
Figure 1B: Courtesy of the Journal of Drugs in Dermatology
http://jddonline.com/articles/dermatology/S1545961615S0042X/4
Figure 1C: Courtesy of the Journal of Drugs in Dermatology
http://jddonline.com/articles/dermatology/S1545961615S0042X/4
Figure 2: Courtesy of the Journal of Drugs in Dermatology
http://jddonline.com/articles/dermatology/S1545961615S0042X/4
Figure 3: Public domain image – Wikipidia Commons
https://commons.wikimedia.org/wiki/Category:Tinea_cruris
Figure 4: Public Domain Image – Wikipidia commons
https://commons.wikimedia.org/wiki/Category:Tinea_capitis#/media/File:4809_lores.jpg
Figure 5: Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, Noronha, Tonita M., Raghavendra S. Tophakhane, and Shobha Nadiger. “Clinico-microbiological study of dermatophytosis in a tertiary-care hospital in North Karnataka.” Indian dermatology online journal 7.4 (2016): 264. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4976403/

