Just as pigmented lesions on the skin can vary widely from freckles to lentigines to nevi to melanoma, similar pigmented lesions can be seen in nails. Melanonychia, brown or black pigmentation in the nail plate, can frequently present a diagnostic challenge for the dermatologist. While most causes of melanonychia are benign, it is important to recognize when the diagnosis is malignant or uncertain.
Dr. Nathaniel Jellinek, president of the Council for Nail Disorders, contributing author to and editor of Scher and Daniel’s Nails, discussed the diagnostic challenge presented by melanonychia during his talk, “Expert Management of Common Nail Problems: Melanonychia” at 2021 ODAC Virtual Conference. He discussed the differential diagnosis of pigmented nail lesions, specific clues to diagnosis, and ultimately, the importance of biopsy to determine the correct diagnosis.
Before we begin, let’s review some definitions of the terminology used by Dr. Jellinek:
Melanonychia : brown or black coloration to the nail plate.
Melanocyte activation: increased pigment production from the nail matrix without melanocytic proliferation; similar to a freckle.
Lentigo: a benign proliferation of single cell melanocytes.
Nevus: benign proliferation of nested melanocytes.
Melanoma: malignant proliferation of melanocytes.
Melanocytes are not the only source of nail pigmentation. Blood, bacteria, fungus, and exogenous material can all cause nail discoloration. These diagnoses also need to be considered in cases of melanonychia. Now let’s get on to Dr. Jellinek’s teaching points.
Use your dermatoscope!
One of the first pieces of advice from Dr. Jellinek when it comes to evaluating melanonychia is to utilize dermoscopy. There are several pigment patterns on dermoscopy that have been identified to be more associated with subungual melanomas than with benign pigmentary lesions. The two features stressed by Dr. Jellinek as especially worrisome are:
Some melanonychia screams “melanoma” from the doorway
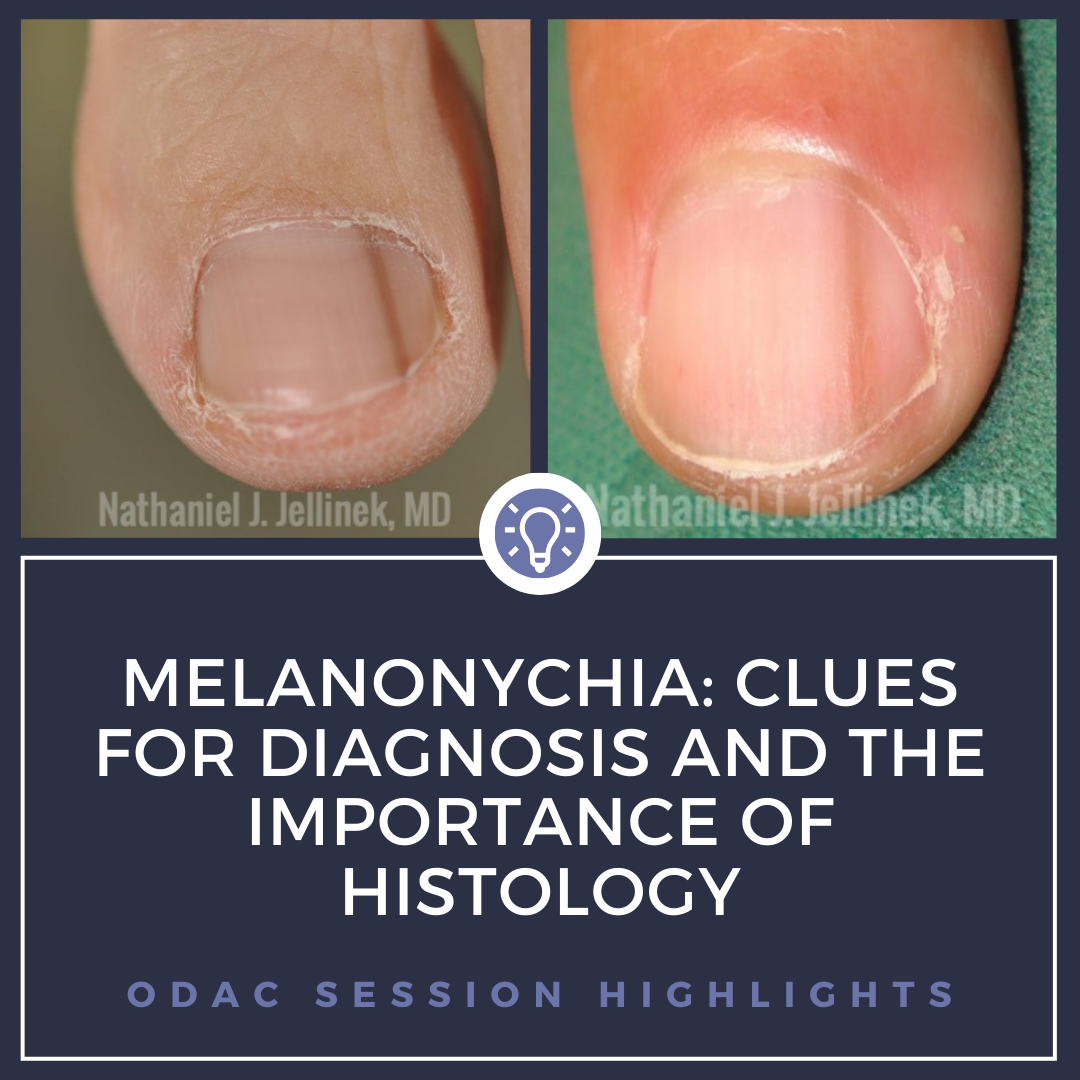
There are times melanonychia is so egregious that it can only be melanoma. A wide, deeply pigmented band with irregular lines and pigmented extension onto the periungual tissues is nearly pathognomonic for melanoma. While it is still important to make sure those cases are biopsied appropriately in the nail matrix and sent for evaluation with experienced dermatopathologists, these are not the cases that serve as a diagnostic challenge. What is concerning is many cases of subungual melanoma look very subtle clinically. Dr. Jellinek provided numerous clinical images of biopsy proven lentigines and nevi as well as melanomas that clinically appear surprisingly similar (See Figure 1). He advised that even with excellent dermoscopy skills and knowledge of nail lesions, ultimately a biopsy is required to make the correct diagnosis. It is critical to recognize when the diagnosis cannot be made clinically or even if there is uncertainty. He argues, there should be a lot of uncertainty due to subtle presentation of earlier subungual melanomas.

Dermoscopy shines for subungual hemorrhage
Subungual hemorrhage is a common benign cause of longitudinal melanonychia and can mimic melanoma to the untrained eye. Dermoscopy shines to diagnose subungual hemorrhage because of the unique features that are often seen. Specific features of hemorrhage include smudged purple or brown blood spots, round proximal shape, filamentous distal shape, and importantly, the lack of background color with linear streaks of pigment. Importantly, as the nail grows, the hemorrhage will spare the proximal nail since the blood is trapped on the ventral surface of the nail plate. In early hemorrhage, it can be more difficult to be certain, and longitudinal follow up of the nail is helpful to see it grow out. Dr. Jellinek recommends photographing all cases of suspected subungual hemorrhage and follow up to ensure it is resolving as expected.
When to worry more
In a review of his personal clinical cases, Dr. Jellinek reviewed images of melanonychia in patients of different phototypes and ages that seemed strikingly similar clinically with very similar dermoscopic features that ultimately had very different histologic findings. Thin pigmented lesions in young patients can still be melanomas, and performing a biopsy is important. However, there are some features that will make you worry more for a malignant cause of melanonychia:
-
- Worry more with wider bands of longitudinal pigment (>2-3mm) is more worrisome, especially in older patients (>65). However, less than 1mm does not get you off the hook!
- Worry more with a solitary pigmented band (i.e. only one nail is involved).
- Worry more with pigment drop out. This refers to areas within the longitudinal band that lack pigment (i.e. streaks of background nail color within the pigmented band).
- Worry more in older patients. However, not all cases of pediatric melanonychia are benign.
- Worry more when you see the triangle sign (i.e., when the pigment is broader proximally than distally). This can be a sign of proliferation.
- Worry more if there is pigment on the periungual skin. Close examination of the skin of the entire affected digit is necessary for evaluation of melanonychia.
Don’t wimp out
So how do you decide how to manage melanonychia? Dr. Jellinek states there are really three possible assessments: some cases are clearly only appropriate for a biopsy, others have enough reassuring features to photo document and monitor (e.g., multiple pigmented nails, classic activation or hemorrhage appearance), and finally, there are all of the cases that fall in the gray zone and cannot be diagnosed clinically. It is important to recognize when you don’t know. It can be helpful to seek a second opinion, but ultimately if there is any uncertainty, a biopsy should be performed. It is important that biopsies are not deferred due to discomfort with nail procedures. Furthermore, biopsies must be performed on the appropriate location (matrix) and provide an adequate tissue sampling for the dermatopathologist. In most instances, the ideal biopsy technique is the matrix shave (tangential excision).
Don’t amputate unless you have to
Historically, subungual melanoma in situ has been treated with amputation as a reflex. However, recent studies show conservative functional surgery for in situ or minimally invasive melanomas have similar outcomes to amputation (Jo G, et al. Functional surgery versus amputation for in situ or minimally invasive nail melanoma: A meta-analysis. J Am Acad Dermatol. 2019 Oct;81(4):917-922). Dr. Jellinek advocates for digit-sparing surgical resection when appropriate due to the associated higher quality of life and supportive data that it is not associated with increased rates of recurrence or disease-specific death.
This information was presented by Dr. Nathaniel Jellinek at the 2021 ODAC Virtual Conference held on January 14-17, 2021. The above highlights from his lecture were written and compiled by Dr. Edita Newton, second-year dermatology resident at the University of Arkansas for Medical Sciences.
Did you enjoy this article? You can find more on Medical Dermatology here.