Perifolliculitis capitis abscedens et suffodiens or dissecting cellulitis (DC) is a rare and chronic disease with a predilection for the occipital, vertex, and parietal scalp. DC is characterized by multinodular lesions with purulent drainage and sinus tract formation. It is classically seen in middle-aged males of African descent. The etiology of the disease is unknown; however, leading theories suggest that stasis associated with follicular occlusion begets bacterial infection and follicular destruction with a subsequent granulomatous and neutrophilic response.1 This is supported by the suppurative nature of the disease and its association with acne conglobota, pilonidal cysts, and hidradenitis suppurativa. These conditions are thought to have a shared etiology and are also widely accepted as being due to follicular occlusion.1 The approach to treatment of DC is varied as there is no current consensus on management. JDD authors Folawiyo Babalola BSA, Margot Chima MD, Ruth Jobarteh MD, and Alice Gottlieb MD PhD present the case of risankizumab, an IL-23 inhibitor, used to successfully treat DC.
INTRODUCTION
CASE
A 65-year-old African American male presented to the dermatology clinic with a 13-year history of recurrent itchy bumps and persistent draining nodules on his scalp- clinical characteristics suggestive of DC. His past medical history was significant for congestive heart failure (ejection fraction of 45%), coronary artery disease, hyperlipidemia, hypertension, and non-alcoholic fatty liver disease. The patient was being followed by our clinic for approximately one year for treatment of recalcitrant DC. He was previously treated with topical clindamycin, doxycycline 100mg BID, intermittent intralesional triamcinolone, chlorhexidine gluconate, fluocinonide, and isotretinoin 30mg BID with minimal response.
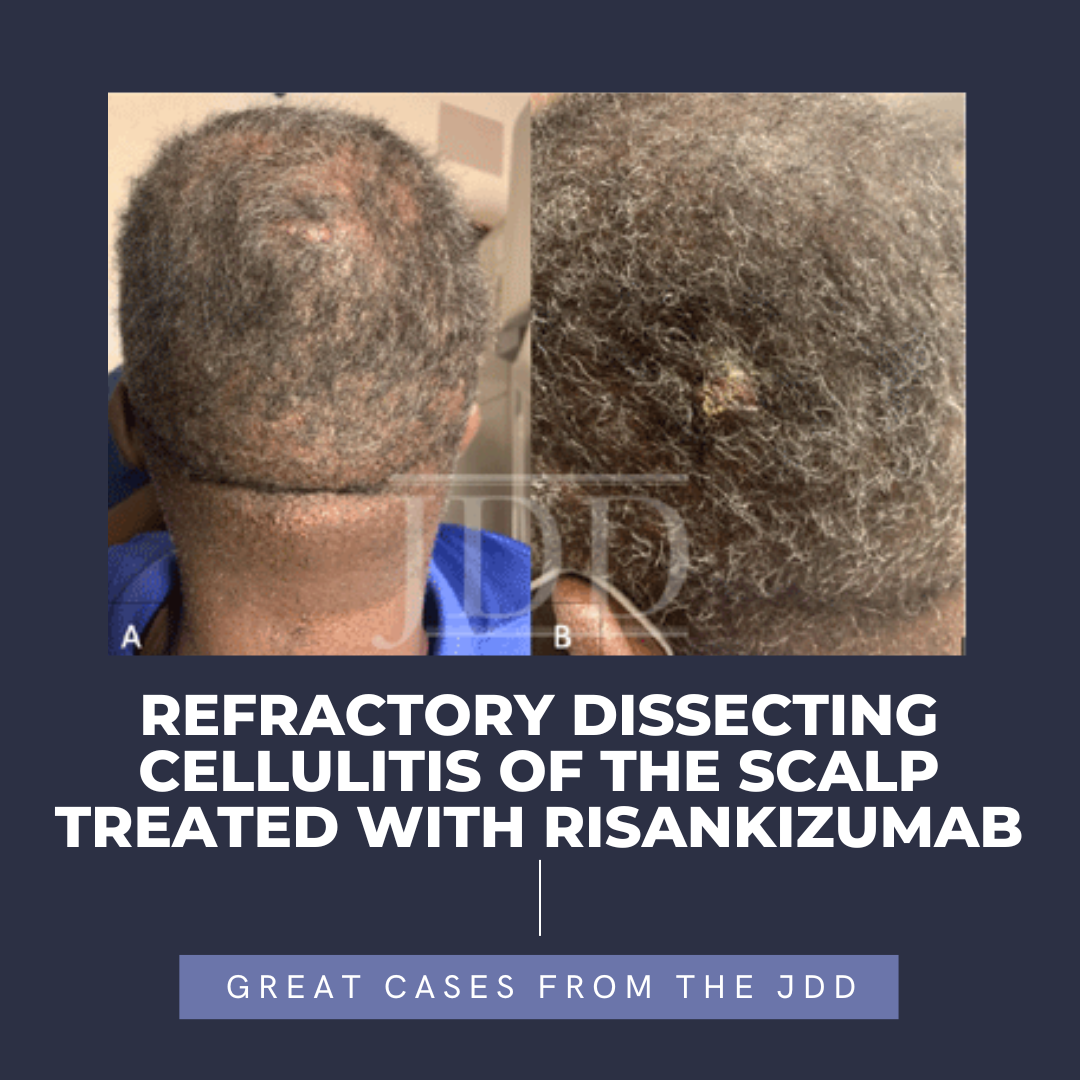
At the time of the visit, the patient reported disease progression. Physical examination showed multiple tender, crusted lesions with suppurative drainage on the parietal and occipital scalp (Figure 1). Due to the inadequate response to previous therapy, and the severe mucocutaneous dryness he experienced on his dose of isotretinoin, we considered starting the patient on concurrent adalimumab. However, the patient’s reduced ejection fraction contraindicated treatment with adalimumab. Alternative therapy considered included secukinumab which was not covered by his insurance.
 The decision was made to start the patient on risankizumab instead. He was initiated at 150mg at weeks 0, 4, and then every 12 weeks. He was discontinued on alternate therapies, including isotretinoin, three months after the initial injection of risankizumab. He presented to the clinic four months after exclusively using risankizumab with an excellent response (figure 2).
The decision was made to start the patient on risankizumab instead. He was initiated at 150mg at weeks 0, 4, and then every 12 weeks. He was discontinued on alternate therapies, including isotretinoin, three months after the initial injection of risankizumab. He presented to the clinic four months after exclusively using risankizumab with an excellent response (figure 2). DISCUSSION
DISCUSSION
There is currently no widely accepted therapeutic guideline for the treatment of DC. The approach to treatment is at the discretion of the physician. However, many physicians initially approach treatment with a trial of oral antibiotics, followed by alternative therapy such as isotretinoin or TNF-alpha inhibitors in recalcitrant cases. Although isotretinoin and TNF-alpha inhibitors are efficacious in treating DC, our patient presented a therapeutic challenge due to his inadequate response to isotretinoin and his contraindication to TNF-alpha inhibitors given his reduced cardiac ejection fraction.
Given the similarity between HS and DC in presentation, we rationalized that the therapeutic approach might also be similar. Some studies have even suggested that DC might be a regional subvariant of HS.7 The efficacy of IL-17 and IL-23 inhibitors in treating HS suggested a possibility of a similar clinical outcome in the treatment of DC. Risankizumab, an IL-23 inhibitor, was first introduced as a novel treatment for psoriasis but has shown efficacy in HS patients.8,9
The rationale for this observed efficacy of IL-23 inhibitors in the treatment of dissecting cellulitis is complex. The selective nature of risankizumab and its proven efficacy in treating DC, as seen in our patient, suggests that IL-23 may play a role in the pathogenesis and treatment of DC. IL-23 is also important in the maturation of Th-17, thus inhibition of IL-23 indirectly decreases levels of IL- 17 and thus should also be considered in the understanding of the drug mechanism of action.10 Consequently, future research should include studies on the efficacy of biologics, especially IL-17 and IL-23 inhibitors in achieving remission and the role of these cytokines in the pathophysiology of DC.
REFERENCES
2. Bolz S, Jappe U, Hartschuh W. Successful treatment of perifolliculitis capitis abscedens et suffodiens with combined isotretinoin and dapsone. J Dtsch Dermatol Ges. Jan 2008;6(1):44-7. doi:10.1111/j.1610-0387.2007.06399.x
3. Brandt HR, Malheiros AP, Teixeira MG, Machado MC. Perifolliculitis capitis abscedens et suffodiens successfully controlled with infliximab. Br J Dermatol. Aug 2008;159(2):506-7. doi:10.1111/j.1365-2133.2008.08674.x
4. Takahashi T, Yamasaki K, Terui H, et al. Perifolliculitis capitis abscedens et suffodiens treatment with tumor necrosis factor inhibitors: A case report and review of published cases. J Dermatol. Sep 2019;46(9):802-807. doi:10.1111/1346-8138.14998
5. Muzumdar S, Parikh S, Strober B. Treatment of refractory dissecting cellulitis of the scalp with guselkumab: Case report. Journal of Dermatology and Dermatologic Surgery. 01/01 2020;24:52. doi:10.4103/jdds.jdds_50_19
6. Schlapbach C, Hänni T, Yawalkar N, Hunger RE. Expression of the IL-23/Th17 pathway in lesions of hidradenitis suppurativa. J Am Acad Dermatol. Oct 2011;65(4):790-798. doi:10.1016/j.jaad.2010.07.010
7. Federico A, Rossi A, Caro G, et al. Are dissecting cellulitis and hidradenitis suppurativa different diseases? Clinics in Dermatology. 2021/02/16/ 2021;doi:https://doi.org/10.1016/j.clindermatol.2021.01.002
8. Huang YW, Tsai TF. A drug safety evaluation of risankizumab for psoriasis. Expert Opin Drug Saf. Apr 2020;19(4):395-402. doi:10.1080/14740338.202 0.1736034
9. Marques E, Arenberger P, Smetanová A, Gkalpakiotis S, Zimová D, Arenbergerová M. Successful treatment of recalcitrant hidradenitis suppurativa with risankizumab after failure of anti-tumour necrosis factor alpha. Br J Dermatol. May 2021;184(5):966-967. doi:10.1111/bjd.19716
10. McGeachy MJ, Chen Y, Tato CM, et al. The interleukin 23 receptor is essential for the terminal differentiation of interleukin 17-producing effector T helper cells in vivo. Nat Immunol. Mar 2009;10(3):314-24. doi:10.1038/ni.1698
SOURCE
Babalola, F., Chima, M., Jobarteh, R., & Gottlieb, A. (2022). Refractory Dissecting Cellulitis of the Scalp Treated With Risankizumab. Journal of Drugs in Dermatology: JDD, 21(3), 313-314.
Adapted from original article for length and style.
Did you enjoy this JDD case report? You can find more here.