Wow! Prior to my attendance to the 2020 Skin of Color Virtual Conference, I had not fully realized the deficits in my learning when it came to recognizing common dermatologic conditions in our skin of color (SOC) patient population. Prior to Dr. Ted Rosen’s lecture on rosacea in SOC patients I had figured I knew enough to identify this dermatologic condition in most clinical settings as well as to formulate a treatment plan. Well, I was proven wrong.
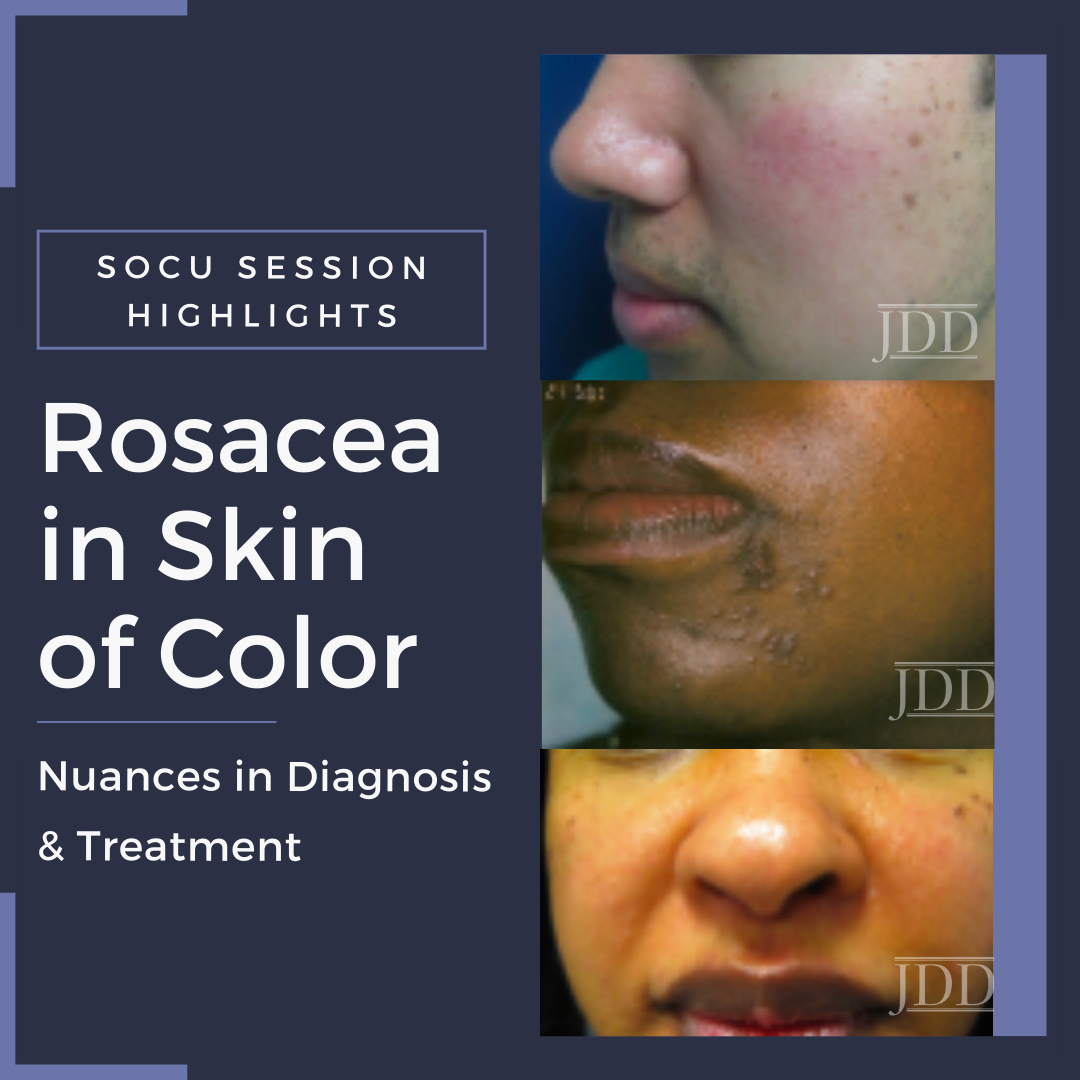
During the Skin of Color Virtual Conference held on September 12-13, 2020, Dr. Rosen provided attendees with a comprehensive lecture titled “Rosacea in Skin of Color Patients.” The lecture highlighted that recognizing rosacea in skin of color patients requires a degree of astuteness that eludes most clinicians due to the lack of studies and information readily available in our most noteworthy print and online publications. The sparsity of treatment guidelines for rosacea in skin of color patients further complicates our ability to confidently tackle this dermatologic condition in a timely manner.
Dr. Rosen’s discussion highlighted a plethora of important tips but the most notable takeaways were:
 Up to 8% of our patients presenting with rosacea are SOC patients and they too oftentimes have the most severe symptoms and debilitating complications
Up to 8% of our patients presenting with rosacea are SOC patients and they too oftentimes have the most severe symptoms and debilitating complications
 How to use common ambulatory techniques and tools such as dermoscopy to assist in diagnosis
How to use common ambulatory techniques and tools such as dermoscopy to assist in diagnosis
 How to implement common treatment options in order to minimize complications such as dyschromia
How to implement common treatment options in order to minimize complications such as dyschromia
While up to 8 percent of patients with rosacea are of SOC, it is still poorly recognized disease in this population. Due to its lack of recognition, there tends to be a broad differential diagnosis when encountering SOC patients with background facial erythema and/or papulo-nodules along the central face. The broad differential spans benign entities such as seborrheic dermatitis and adult acne to complex diseases such as systemic lupus erythematosus and dermatomyositis. Here is a quick way to help differentiate among these cutaneous diseases:
-
- Seborrheic Dermatitis: identify concomitant involvement of the scalp, eyebrows and ears. Take note for the presence of greasy scale
- Adult Acne: identify comedones!
- Systemic Lupus Erythematosus: malar erythema is usually a diffuse erythematous patch across the nasal bridge and cheeks that spare the melo-labial creases
- Dermatomyositis: ask about generalized or muscle weakness. Take note of other dermatologic manifestations such as poikiloderma, photosensitizing rash across sun exposed skin, gottren papules.
- Allergic Contact Dermatitis: identify any preceding application of topical agent or potential airborne exposures. Ask about possible pruritus!
- Sarcoidosis: papules-nodules are usually more firm yellow-brown in color without background erythema or presence of telangiectasia
The importance of a comprehensive history cannot be emphasized enough! Ask patients when do their cutaneous symptoms worsen? Can they identify specific rosacea triggers such as heat, sweat or intake of spicy foods? What products have they used? Do these products improve or worsen their condition? And to help guide our thought processes a thorough review of systems can help to elucidate the presence of systemic symptoms.
During your physical exam, don’t shy away from using the amazing techniques our mentors have taught us or the handy dermatoscope in our white coat pocket. The use of diascopy or dermoscopy to help highlight telangiectasias can point us towards a diagnosis of rosacea. Also being able to identify non-comedonal papules can be helpful to assist with differentiating it from another common entity, acne. And look elsewhere! Inspect the scalp, eyebrows, ears, trunk and upper extremities including the hands and nails. As we all know-cutaneous manifestations is an important clue to systemic diseases. Here is a quick list of the classic features of rosacea in SOC patients:
-
- Background erythema
- Telangiectasias
- NON-comedonal papules
Once rosacea is recognized in SOC patients-treat promptly. Complications such as dyschromia, post-inflammatory hyperpigmentation and even rhinophyma can be debilitating to most patients.
Rosacea Treatment Options to Consider
-
- Topical therapies
- Azelaic Acid
- Metronidazole
- Ivermectin
- Minocycline (foam formulation is now available)
- Sodium Sulfacetamide/Sulfur
- Oxymetazoline
- Brimonidine
- Systemic therapies
- Tetracycline Antibiotics (example: Doxycycline)
- Azithromycin
- Ivermectin
- Physical Modalities
- Laser (***use cautiously in SOC patients due to potential adverse effect profile)
- Topical therapies
For the general dermatologist, keep in mind that most topical remedies help to reduce associated erythema and/or dyschromia and not as much for the treatment of the papular variant of rosacea.
The key to minimizing the morbidity and complications associated with rosacea is employing oral therapies prior to the onset of dyschromia, post inflammatory hyperpigmentation and rhinophymatous changes to the nose.
While recommending products and treatment options is extremely helpful to patients, it is equally important to reiterate products to avoid! The following products should be avoided in all individuals who have rosacea:
-
- Astringents
- Exfoliators
- Alcohol based cleansers
- Exotic cosmetics
- Chemical sunscreens
- ANY product that stings or causes irritation post-application
In summary, prompt recognition of rosacea in SOC patients is extremely important. Not only does it instill trust in our patients to be able to recognize common cutaneous diseases in SOC patients, just as importantly, we can help minimize long term sequelae of dyschromia and post-inflammatory hyperpigmentation. Furthermore, our patients seek relief and as dermatologists we are uniquely qualified to provide a diagnosis and a comprehensive treatment plan.
This information was presented by Dr. Ted Rosen at the Skin of Color Virtual Conference held September 12-13, 2020. The above highlights from his lecture were written and compiled by Dr. Freba Farhat.
Clinical images used with permission from the Journal of Drugs in Dermatology.
you enjoy this article? Find more on Skin of Color here.