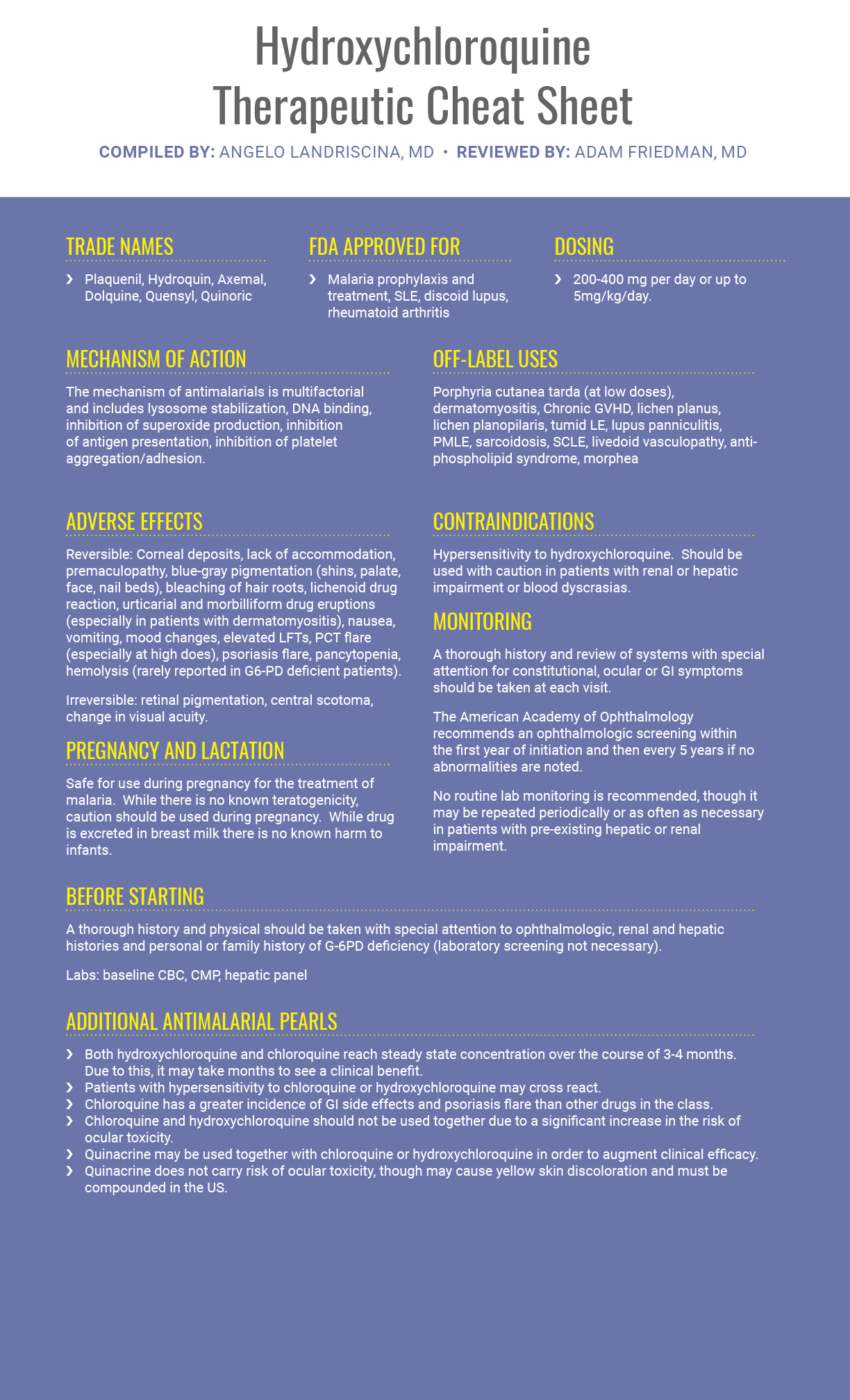
Welcome back to another installment of Therapeutic Cheat Sheet – the series where we break down complex therapeutics into an easy-to-use reference. This month, we turn our focus to hydroxychloroquine and other antimalarials. While this versatile class of drugs has been in use for decades, recent updates to monitoring recommendations have made their use easier than before. Here’s what you need to know about hydroxychloroquine.
Further Reading
If you would like to read more about hydroxychloroquine, check out the following articles published in the Journal of Drugs in Dermatology
Trends in the Outpatient Medication Management of Lupus Erythematosus in the United States
BACKGROUND: Systemic lupus erythematosus (SLE) and chronic cutaneous lupus (CCLE) therapy has changed little over the past 50 years. In March 2011, the US Food and Drug Administration (FDA) approved belimumab, complementing the three preexisting approved therapies: low dose aspirin, prednisone, and hydroxychloroquine.
OBJECTIVE: The objectives for this study were to evaluate trends in the medications prescribed for the management of lupus erythematosus (LE) and to assess how treatment varies among different specialists.
METHODS: Outpatient visits for treatment of lupus and its comorbidities were identified in the National Ambulatory Medical Care Survey (NAMCS), a representative survey of visits to physician offices in the United States. Data was evaluated to determine patient demographics, treatments prescribed by each specialty, and comorbidities encountered during the study period of 1993-2010.
RESULTS: From 1993-2004, prednisone was the most frequently prescribed medication; however, prednisone became the second most frequently prescribed medication in 2005-2010, as hydroxychloroquine became the leading medication prescribed for LE. In primary care physicians and other non-dermatology specialists, the most frequently prescribed medications for lupus were prednisone and hydroxychloroquine; whereas, hydroxychloroquine and triamcinolone were the top two medications preferred by dermatologists.
LIMITATIONS: The NAMCS collects cross-sectional data, such that individual patients cannot be followed over time. Hence, it does not provide data regarding the incidence of disease, patient age at the time of diagnosis, change in individual patient’s medication regimens over time, or prognosis related to patient demographics. In addition, it is possible that the physician did not always record nonprescription medication use, such as NSAIDS, since these are typically used first line.
CONCLUSION: First-line treatment of LE changed minimally from 1993 to 2010, with prednisone and hydroxychloroquine serving as the primary medications utilized by most physicians for the management of LE.
Successful Treatment of Perniosis With Hydroxychloroquine
Background: The current medical therapies for perniosis are diverse. The agents used have produced variable results and lack evidence-based data. Objective: To determine outcomes of patients with perniosis treated with hydroxychloroquine. Methods: In this retrospective study, patients with a diagnosis of perniosis treated with hydroxychloroquine were analyzed for dosage required, subjective improvement in signs and symptoms, and adverse drug reactions. Results: Hydroxychloroquine resulted in improvement of symptoms in four of five patients. Review of the literature has revealed 12 out of 51 cases have responded to hydroxychloroquine alone or in combination with other therapies. Conclusion: Hydroxychloroquine is a relatively safe, well tolerated alternative therapy for the treatment of perniosis and should be considered as part of the initial management. Additional data are needed to further evaluate this drug in a prospective manner and in a larger population of patients.
![]() Rhabdomyolysis Associated with Quinacrine Therapy in a Patient with Chronic Cutaneous Lupus Erythematosus
Rhabdomyolysis Associated with Quinacrine Therapy in a Patient with Chronic Cutaneous Lupus Erythematosus
We describe a patient who developed rhabdomyolysis 6 weeks after starting combination therapy with hydroxychloroquine and quinacrine for the treatment of chronic cutaneous lupus erythematosus (CCLE). Myopathy due to 4-aminoquinolone antimalarials has been well documented. It is plausible that quinacrine may induce muscle injury in a manner similar to other antimalarials but, to our knowledge, rhabdomyolysis associated with antimalarial therapy has not been reported.
Did you enjoy this Therapeutic Cheat Sheet? Find more here.

