Psoriasis involves a complex inflammatory cascade mediated by various cytokine effectors. Over the past fifteen years, treatment options have evolved to include biologic medications that provide targeted inhibition of various pathways. IL-23 has emerged as an important inflammatory cytokine in the pathogenesis of psoriasis. We continue our series, Therapeutic Cheat Sheet, with a closer look at IL-23 inhibitors.
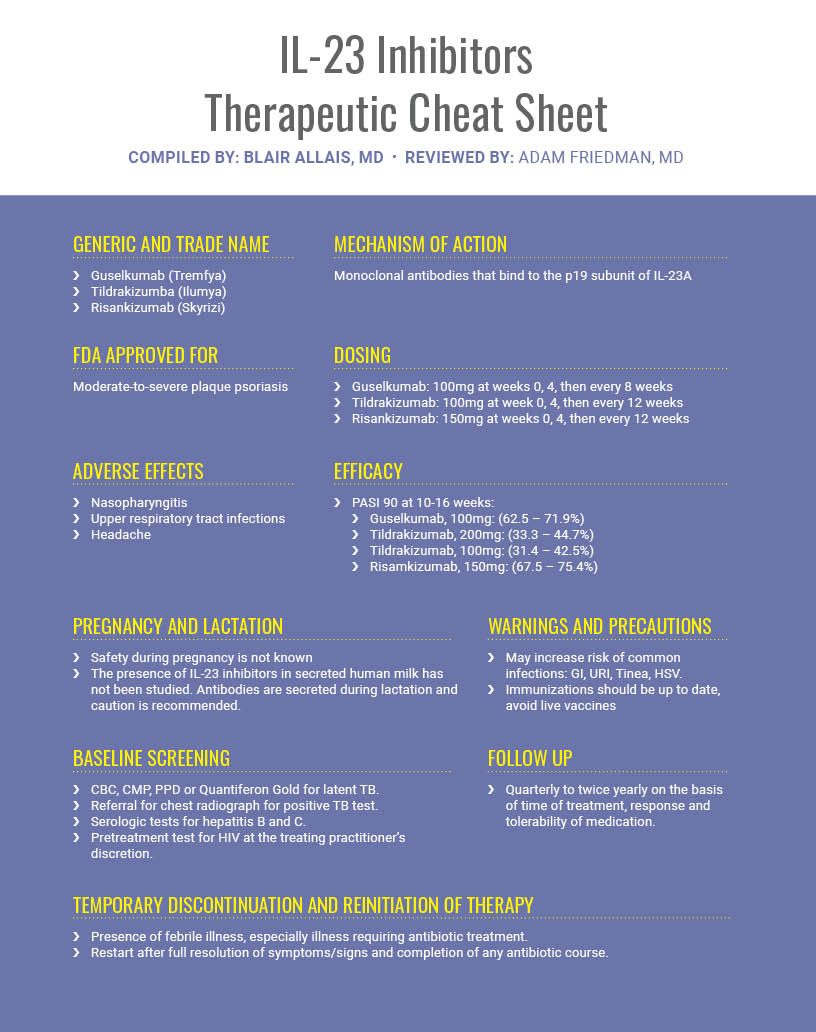
Overall, IL-23 inhibitors have demonstrated superior efficacy and safety in the treatment of psoriasis. The relatively infrequent dosing is ideal with regard to maintaining adherence. Ultimately long term effects of this class of biologics still need to be monitored through post-marketing surveillance and further research. If you would like to read more about IL-23 inhibitors, check out the following 2 articles published in the Journals of Drugs in Dermatology:
 IL-23 Versus IL-17 in the Pathogenesis of Psoriasis: There is More to the Story Than IL-17A
IL-23 Versus IL-17 in the Pathogenesis of Psoriasis: There is More to the Story Than IL-17A
April W. Armstrong MD MPH, Charlotte Read MBBS BSc, Craig L. Leonardi MD, Leon H. Kircik MD
ABSTRACT
Our understanding of psoriasis pathogenesis has evolved considerably. Cytokines within the TH1 and TH17 pathways have been found to be critical in psoriasis immunopathology. The TH17 pathway, which is centered around the interplay between IL-23 and IL-17, is now known to be at the core of psoriasis immune dysregulation. IL-23 acts as a key regulator of the TH17 pathway. Therapies targeting either IL-23 or IL-17 have shown great efficacy in psoriasis and have helped augment our understanding of psoriasis pathogenesis. Therapies such as ustekinumab and guselkumab inhibit IL-23. Ustekinumab targets the p40 subunit common to both IL-23 and IL-12 while guselkumab targets the p19 subunit found in IL-23. IL-17 subtypes trigger downstream inflammation in psoriasis. In particular, IL-17A, IL-17F, and IL-17C are elevated in psoriatic lesions; with IL-17F and IL-17C more elevated than IL-17A. Therapies such as secukinumab, ixekizumab, and brodalumab inhibit IL-17 subtypes. For example, brodalumab inhibits the downstream effects of all five IL-17 subtypes (IL-17A, IL-17AF, IL-17F, IL-17C, and IL-17E) via IL-17 receptor blockade; brodalumab can also normalize the levels of IL-23. Therefore, using a receptor-blocking therapy, such as brodalumab, that can act on multiple inflammatory cytokines, both IL-17 and IL-23 can be suppressed.
In this paper, we describe the importance of the TH17 pathway in psoriasis pathogenesis with a focus on the roles of IL-23 and IL-17 within this pathway. We also discuss the different IL-17 subtypes involved in psoriasis immunopathology and the multitude of cells that can produce these subtypes. Finally, we examine treatments that inhibit IL-23 and IL-17.
 Long-Term Efficacy of Guselkumab for the Treatment of Moderate-to-Severe Psoriasis: Results from the Phase 3 VOYAGE 1 Trial Through Two Years
Long-Term Efficacy of Guselkumab for the Treatment of Moderate-to-Severe Psoriasis: Results from the Phase 3 VOYAGE 1 Trial Through Two Years
Christopher E.M. Griffiths MD, Kim A. Papp MD, Alexa B. Kimball MD, Bruce Randazzo MD, Michael Song MD, Shu Li PhD, Yaung-Kaung Shen PhD, Andrew Blauvelt MD
ABSTRACT
Background: Due to the chronic nature of psoriasis, it is important to assess the sustained response of treatments over time. Objective: To assess the efficacy of continuous treatment with guselkumab (an interleukin-23 blocker) through two years in the phase 3 VOYAGE 1 trial. METHODS: Patients were randomized to placebo, guselkumab, or adalimumab at baseline. Placebo-randomized patients crossed over to guselkumab at week 16 (placebo→guselkumab) and adalimumab-randomized patients crossed over to guselkumab at week 52 (adalimumab→guselkumab); all patients received open-label guselkumab beyond week 52. Efficacy was assessed based on the Psoriasis Area and Severity Index (PASI; proportion of patients achieving ≥75%, 90%, or 100% improvement [PASI 75/90/100]) and the Investigator’s Global Assessment (IGA; proportion achieving nearly clear [IGA 0/1] or completely clear [IGA 0]). As pre-specified, efficacy data were analyzed using non-responder imputation (NRI; patients with missing data counted as non-responders) after applying treatment failure rules (TFR; patients meeting TFR counted as non-responders thereafter) through week 48 and by applying TFR only from week 52 through 100. All endpoints were also analyzed using NRI and As Observed methodology for the guselkumab group through week 100. RESULTS: The clinical responses were maintained through week 100 based on all three analyses. Based on pre-specified analyses, proportions of patients who achieved PASI 75, PASI 90, PASI 100, IGA 0/1, and IGA 0 were 94.8%, 82.1%, 49.0%, 82.4%, and 53.8%, respectively, at week 100. Results were similar for the placebo→guselkumab and adalimumab→guselkumab groups at week 100. As expected, proportions of patients achieving these endpoints were similar based on As Observed analyses and slightly lower when the more conservative NRI rules were applied. CONCLUSIONS: High levels of efficacy were maintained through two years of continuous treatment among guselkumab-treated patients, and efficacy improved through two years among adalimumab-treated patients who crossed over to guselkumab at one year.
References
- Armstrong AW, Puig L, Joshi A, et al. Comparison of Biologics and Oral Treatments for Plaque Psoriasis: A Meta-analysis . JAMA Dermatol.2020;156(3):258–269. doi:10.1001/jamadermatol.2019.4029
- Menter, A et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. Journal of the American Academy of Dermatology. 2019; 80(4): 1029-1072.
- Lee EB, Amin M, Wu JJ. Interleukin 23 Inhibitors. In: Wolverton, SE, Wu, JJ, eds. Comprehensive Dermatologic Drug Therapy. 4th Philadelphia, PA: Elsevier; 2021.
Did you enjoy this therapeutic cheat sheet? You can find more here.