CASE REPORT
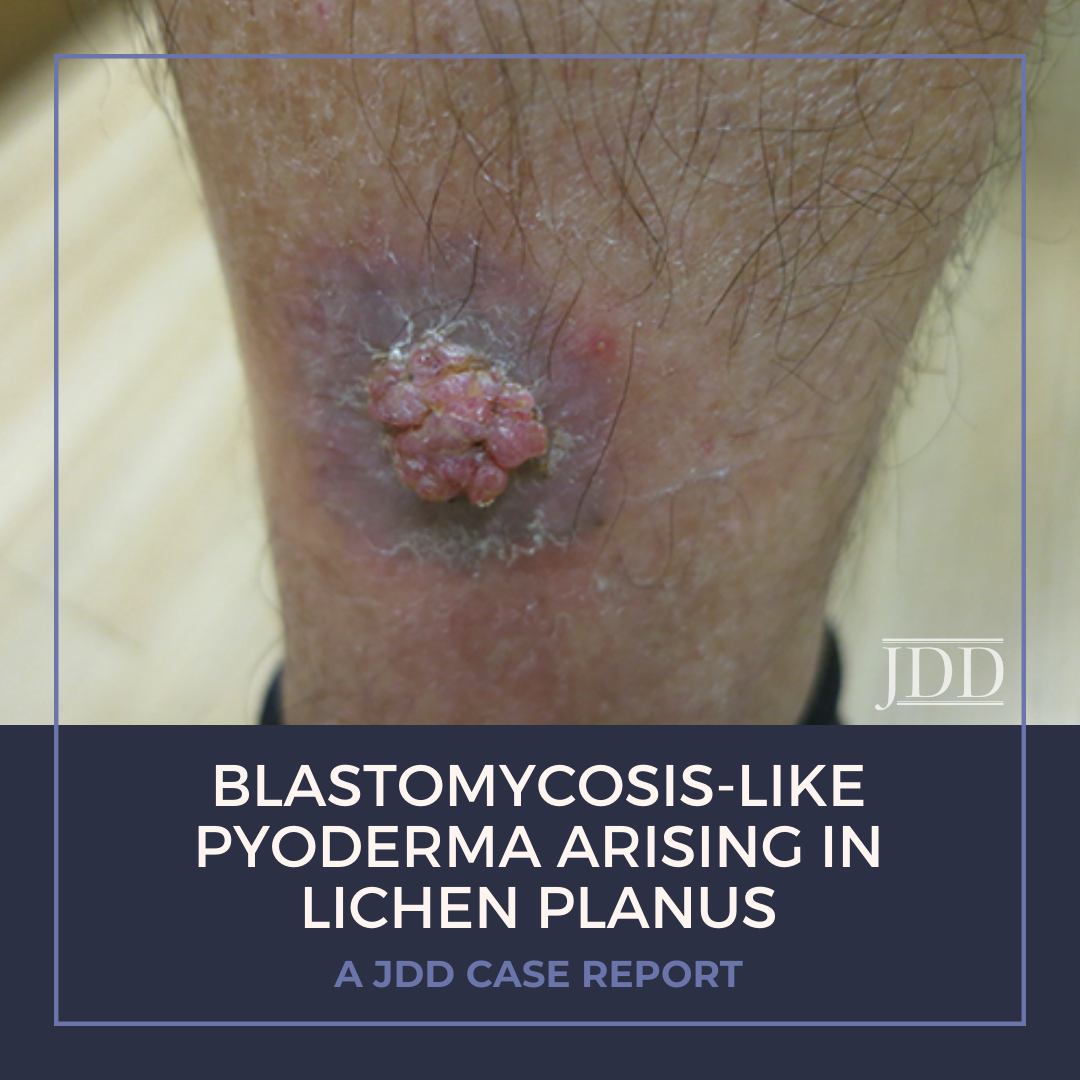
A 71-year-old Fitzpatrick phototype IV man with a history of hyperlipidemia and extensive travel to the Middle East presented with a mildly painful vegetative growth on his right lower leg for 1.5 months (Figure 1). In 2014, the patient reported a pruritic “rash” in the same location, which was treated with fluocinonide .05% ointment with resolution.
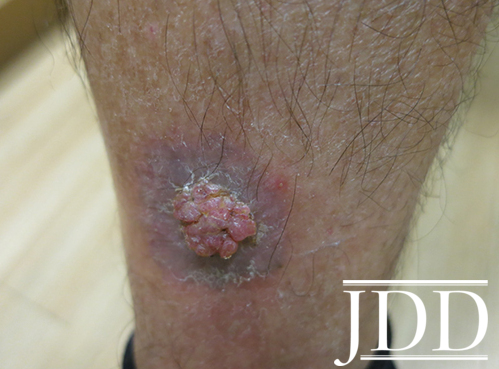
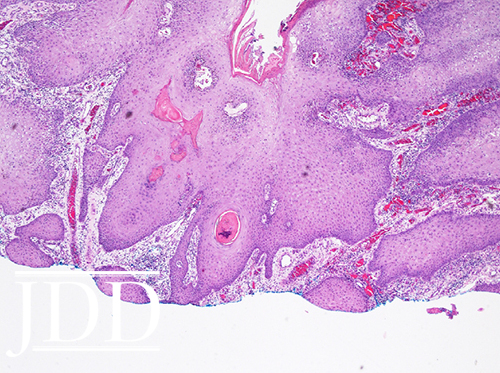
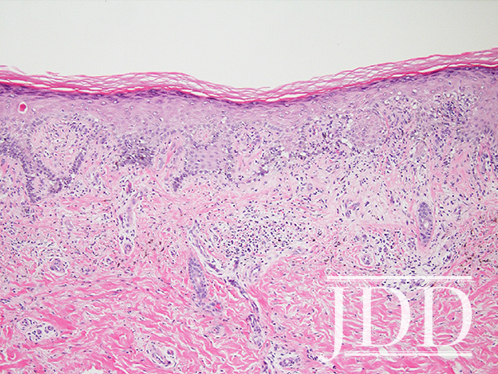
Physical examination revealed a well-circumscribed violaceous scaly plaque with a central exophytic cerebriform soft nodule. Histopathological examination of a shave biopsy revealed papillated and endophytic acanthosis with hyperkeratosis, neutrophilic inflammation, and congested granulation tissue (Figure 2). A punch biopsy from the plaque demonstrated a vacuolar interface and mild superficial perivascular dermatitis with acanthosis and dermal hemosiderin deposition, most consistent with hypertrophic lichen planus (Figure 3). Tissue cultures, PAS, and T. pallidum immunostains were negative. Taken together, these features were suggestive of blastomycosis-like pyoderma arising in lichen planus.
Following biopsy, the patient was treated with topical steroid clobetasol cream and the lesion resolved with post-inflammatory pigment alteration.
DISCUSSION
Blastomycosis-like pyoderma (BLP) is a rare reactive skin disease that results from an exaggerated immunological response to a prolonged inflammatory milieu. Historically, it arises in the setting of bacterial infection with Staphylococcus aureus, Pseudomonas aeruginosa, and β-hemolytic streptococci as the most frequently implicated microorganisms. BLP typically affects the elderly and otherwise immunocompromised patients, though there is evidence that it can occur in normocompetent individuals, as seen with our patient.1 Clinically, patients with BLP present with large, crusted, verrucous plaques with pustules and well-defined and raised borders. Although the etiology is unknown, it was postulated that acute inflammatory responses induce localized neutrophilic infiltrates that release connective tissue-activating peptides and trigger the rapid production of glycosaminoglycans, found in ground substance and fibroblasts. This flourish of connective tissue elongates dermal papillae, which support a larger germinative cell volume producing the pseudocarcinomatous hyperplasia seen in BLP.2 Pseudocarcinomatous hyperplasia, a common histological feature of BLP, can mimic an epithelial neoplasm like squamous cell carcinoma (SCC), making this entity both clinically and pathologically challenging. This highlights the necessity for a tissue diagnosis both to identify infectious agents and rule out malignancy when confronted with BLP. Treatment for BLP includes antibiotics to which cultured organism(s) is/are sensitive, intralesional corticosteroids, acitretin, surgical excision, or local ablative measures.3
Interestingly, infection was not the causative factor but rather a primary inflammatory disease. Lichen planus (LP) is a chronic inflammatory papulosquamous dermatosis that is historically characterized by pruritic, polygonal, flat-topped, violaceous papules and plaques, however numerous atypical presentations have been reported ranging from annular/atrophic to bullous.4 In line with the discussion above, SCC has been reported in oral LP, and also, though less commonly, in cutaneous LP.5 There are several reported cases in which SCC arose in hypertrophic cutaneous LP located on lower limbs.6 In BLP, a chronic inflammatory insult induces squamous cell proliferation in a manner that can mimic SCC.7 However, these changes are hyperplastic rather than neoplastic. Due to the increased risk of SCC, tissue should be obtained to rule out malignancy in the setting of a newly evolving lesion in lichen planus.
LP has classically been associated with the Koebner isomorphic phenomenon, defined by lesions of an existing condition that appear at previously unaffected sites, secondary to trauma. This report of BLP arising in LP, however, describes a new primary lesion at the site of an existing LP plaque, more fitting of Wolf’s isotopic response, or the development of a new dermatologic finding in a region previously affected by another unrelated skin disease.8 Though rare, BLP arising in a primary inflammatory disease has been described; Cecchi et al. reported a patient with BLP arising in chronic vesicular hand eczema.1 The etiology of Wolf’s isotopic reaction is unclear, though both immunologic and neurohormonal pathogenicities have been proposed. The immunologic hypothesis suggests that an existing condition may lead to changes in the regional immune system, with the development of intraepidermal memory T-cells that can later be triggered to induce a new condition.9 The neurohormonal hypothesis suggests that damaged nerve fibers release neuropeptides that alter the immune system and initiate favorable conditions for a new disease.10 In this case, inflammation from the patient’s existing LP lesion may have altered the local immune response to produce connective tissue that laid the dermal foundation to support BLP growth.
Here, a unique presentation of a rare hyperproliferative reactive process is reported: BLP arising in LP, likely resulting from Wolf’s isotopic response. Given the breadth of differential diagnoses, tissue obtained for histopathology and cultures are necessary to rule out an array of imitators and direct appropriate treatment.
Source:
Stephanie Kao BA, Ramsin Yadgar BS, Thomas Enelow MD, Adam Friedman MD, (2017). Blastomycosis-like Pyoderma Arising in Lichen Planus. Journal of Drugs in Dermatology, 17(2), 233-235.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this case report? Find more here.